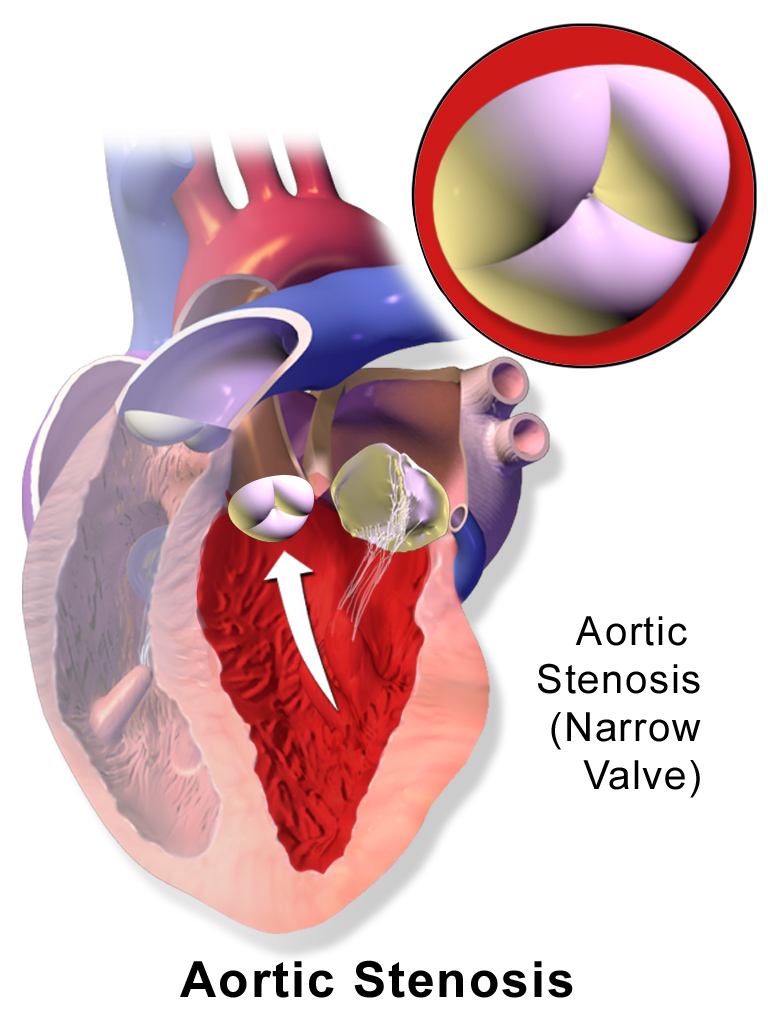
Aortic stenosis describes a narrowing of the aortic valve which can occur for various reasons.
Pathophysiology
- The aortic valve is one of the two semilunar valves in the heart and is found between the left ventricle and the aorta. It has three valve leaflets which are the anterior, left and right leaflets.
- In aortic stenosis, there is a stenosis i.e., narrowed opening of the aortic valve, meaning it’s harder for blood to leave the left ventricle during systole.
- This reduces the stroke volume, and in turn, cardiac output.
- This increases the pressures inside the left ventricle.
- Over time, there is left ventricular hypertrophy in attempts to maintain adequate stroke volumes.
- Eventually, this left ventricular hypertrophy starts to cause impaired filling of the heart in diastole due to reduced compliance and relaxing of the heart.
- With time, patients can develop heart failure if the heart cannot meet the physiological demands of the body.
BruceBlaus, CC BY 3.0 , via Wikimedia Commons
Aortic Stenosis
Causes
- Calcific aortic valvular disease: This is the most common cause of AS and tends to occur in older patients. You can sometimes see a calcified valve on a chest x-ray in these patients.
- Congenital bicuspid aortic valve: This increases the risk of developing calcification of the valve
- Rheumatic heart disease: Due to destruction of the valve secondary to autoimmune destruction of the valve
- Infective endocarditis: Vegetations on the valve
Clinical Features
Symptoms of AS are largely related to a reduced cardiac output, as it is more difficult to get blood out of the stenosed valve. Thus, you get;
- Syncope
- Angina: Reduced cardiac output, increased oxygen demand from a hypertrophied myocardium, and compression of coronary vessels due to ventricular hypertrophy
- Dyspnoea
- Pre-syncope
- Symptoms worsen on exertion
- Features of heart failure if cardiac output cannot maintain the physiological needs of the body e.g.
- Paroxysmal nocturnal dyspnoea
- Orthopnoea
- Left ventricular heave: Due to left ventricular hypertrophy
- Aortic thrill: Thrills are vibrations which can be felt over areas of turbulent blood e.g. heart murmurs.
- Narrow pulse pressure: Difference between systolic and diastolic blood pressure will be small.
- Slow-rising pulse: Slower rate of ejection of blood.
- Low pulse volume: Due to a smaller stroke volume.
- Pulse parvus et tardus: Combination of the above two, just in Latin (pulse parvus = low volume, et tardus = delayed)
Auscultation
- S1 is the sound you hear from the atrioventricular valves closing (mitral and tricuspid). It indicates the start of systole.
- S2 is the sound you heart from the closing of the aortic and pulmonary valves. It indicates the start of diastole. S2 itself is made up of A2 and P2 – closure of the aortic and pulmonary valves respectively. A2 happens first, then P2.
Aortic Stenosis Murmur
- Crescendo-decrescendo:
- Gets louder and then gets softer.
- This is because blood moves slowly through the stiff valve at first, but does eventually start to get through. This is the crescendo part.
- As the heart begins to relax, less blood flows through the valve, thus the sound gets quieter.
- Hence the sound will get louder, and then quieter.
- Ejection systolic murmur: You’ll hear this murmur at the same time as systole. In practice, the pulse can be palpated during auscultation. The murmur should be at the same time as the pulse as that signifies systole.
- Ejection click: May be audible. Represents the stenotic valve clicking open
- Bilateral radiation to the carotids: The carotid arteries are anatomically linked to the aorta
- Louder on expiration
- S4 sound: This sound occurs just before S1 i.e. just before systole. It’s the sound of turbulent blood flow going from the left atrium into a stiff and hypertrophied left ventricle.
- Quieter S2: As S2 represents the closing of both aortic and pulmonary valves, if the aortic valve is less mobile, it won’t close as forcefully as normal resulting in a quieter S2.
Investigations
Bedside
- ECG: Features of left ventricular hypertrophy or left axis deviation
Bloods
- FBC: Patients may develop a microangiopathic haemolytic anaemia (MAHA) due to lysis of RBCs as they pass through the narrowed valve, so you may see anaemia. Schistocytes may be seen on blood film - these are essentially fragmented red blood cells.
- BNP: To look for heart failure
Imaging
- Chest X-ray:
- Left ventricular hypertrophy
- May visualise a calcified aortic valve
- Features of heart failure e.g. cardiomegaly/pulmonary oedema
- Echocardiogram: This is the mainstay of diagnosis. It allows visualisation of the aortic valve function as well as assessing for any signs of left ventricular hypertrophy/heart failure.
Differential Diagnosis
- Mitral regurgitation
- Hypertrophic cardiomyopathy
- Aortic sclerosis: This is thickening, but no narrowing, of the aortic valve due to age related calcification.
Management
- Surgical Aortic Valve Replacement (SAVR): Involves open surgery to replace the valve
- Transcatheter Aortic Valve Implantation/Replacement (TAVI/TAVR): This is where the valve is replaced via a catheter which is usually inserted into the femoral artery, thus negating the need for open surgery.
Tissue vs Mechanical Valves
- A decision would have to be made between a tissue valve or mechanical valve and this would depend on various factors, including if the patient is suitable for anticoagulation.
- A tissue valve wouldn’t require anticoagulants, whilst a mechanical valve will require lifelong anticoagulation with warfarin.
- Furthermore, tissue valves last around 10-20 years whilst mechanical valves will last longer.
Complications
- Heart failure
- Angina
- Arrhythmias
References
https://www.lhch.nhs.uk/media/1497/e3154_as_educationbrochure_english.pdf
https://academic.oup.com/eurheartj/article/38/36/2739/4095039#115331374
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/replacement-heart-valves
https://www.med.ucla.edu/wilkes/Systolic.htm
https://www.med.ucla.edu/wilkes/S4.htm
https://www.msdmanuals.com/professional/hematology-and-oncology/anemias-caused-by-hemolysis/traumatic-hemolytic-anemia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6654225/
https://stanfordmedicine25.stanford.edu/the25/cardiac.html
https://www.nice.org.uk/guidance/ipg78/chapter/1-Guidance