Infection and inflammation of the middle ear, usually preceded by a viral upper respiratory tract infection.
Pathophysiology
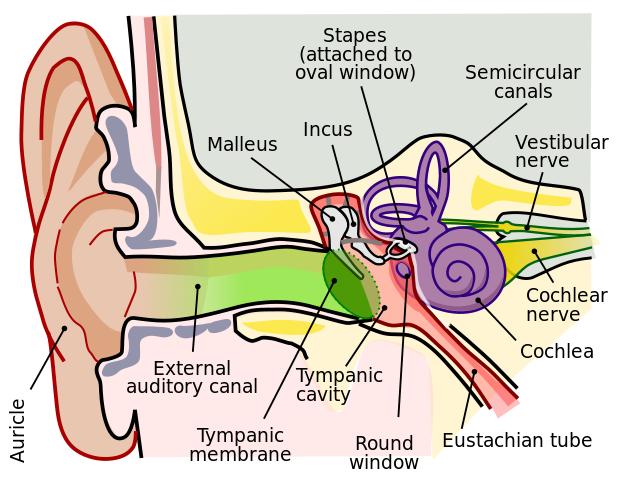
- The Eustachian tube connects the middle ear to the nasopharynx. It is crucial for draining middle ear secretions, as well as allowing equalisation of pressure.
- Otitis media is usually preceded by a viral upper respiratory tract infection. This can result in inflammation and oedema of various structures, including the nasal mucosa and nasopharynx.
- Ultimately, this causes Eustachian tube dysfunction and can result in a negative pressure forming in the middle ear.
- This negative pressure essentially pulls bacterial/viral pathogens into the middle ear from the nasopharynx.
- Furthermore, any blockage of the Eustachian tube i.e. secondary to an infection, can result in fluid stagnating in the middle ear which subsequently is more prone to becoming infected.
- Additionally, these preceding viral infections can alter the mucosal immunity and changing surface antigens that encourage adherence of bacteria.
- Children, particularly those <1 year, have shorter, more horizontal, and wider Eustachian tubes, increasing their risk of developing otitis media.
Lars Chittka; Axel Brockmann, CC BY 2.5 , via Wikimedia Commons
Middle Ear Anatomy
Risk Factors
- Craniofacial abnormalities that result in Eustachian tube dysfunction e.g. cleft palate
- Down’s syndrome: Due to abnormal mucosa and reduced immunity
- Primary ciliary dyskinesia: Due to reduced mucus clearance
- Tobacco smoke exposure
- Bottle feeding (breastfeeding is protective)
- History of atopy
- Day care attendance: Due to increased infection risk
- Family history
Causes
- Bacterial causes: The following microbes account for approximately 95% of otitis media
- Streptococcus pneumoniae
- Haemophilus influenza
- Moraxella catarrhalis
- Streptococcus pyogenes
- Viral causes: Influenza, rhinovirus, RSV, adenovirus
Clinical Features
- Otalgia
- Rubbing/pulling of the ear
- Fever
- Change in behaviour: Otitis media is more common in younger children/babies, so symptoms may be less specific. For example:
- Reduced feeding
- Restlessness
- Crying
- Otoscopy
- Bulging of the tympanic membrane
- Erythematous/cloudy/yellow tympanic membrane
- Acute suppurative otitis media:
- You may be able to see an air-fluid level behind the tympanic membrane.
- Patients might complain of increasing pain in the ear, followed by discharge – this usually happens where there has been a perforation of the tympanic membrane.
- Patients might feel a pop when this occurs.
Differential Diagnosis
- Otitis externa: Will not involve the tympanic membrane, and the external auditory canal will be the main site of pathology.
- Myringitis: Erythema and vessel injection of the tympanic membrane only i.e. inflammation of the tympanic membrane alone. The middle ear is unaffected here.
- Otitis media with effusion: Also known as glue ear – a chronic condition without signs of acute infection.
Management
Admission
- Patients with severe infection and systemic involvement.
- People with complications of otitis media.
- <3 months with temperature >38 (can consider admission in patients <3 months or patients 3-6 months with temperature >39).
Conservative
- Analgesia
- Safety-netting: Not all patients require antibiotics, so safety-netting with regards to worsening symptoms, systemic involvement, or no symptom improvement after 3 days is important (the usual course of otitis media is 3 days but it can last for 1 week)
Medical
- Oral antibiotics
- First line: 5-7 days amoxicillin, or clarithromycin/erythromycin in patients who are penicillin allergic.
- Second line: 5-7 days of co-amoxiclav if patients have no symptom improvement within 2-3 days of taking the first-line antibiotic.
Complications
- Facial nerve palsy
- Tinnitus
- Otitis media with effusion
- Mastoiditis: Infection of the mastoid air cells - these patients will be very unwell and present with a boggy swelling of the mastoid process.
- Meningitis
- Intracranial abscess
Otitis Media with Effusion (OME)
- Also known as glue ear; occurs when the middle ear becomes fluid filled. In this scenario, there are no signs or symptoms of acute infection/inflammation.
- It results in hearing loss.
- On examination, the ear drum may have an abnormal colour, and it is possible to see bubbles or an air-fluid level as well. The ear drum may also be retracted, as opposed to bulging.
- Initially, patients can be monitored for a 3-month period, as OME can often resolve on its own.
- Hearing aids may be offered to patients with bilateral OME and hearing loss, if surgery is not possible/contraindicated.
- The surgical intervention for OME is a myringotomy (creating a small hole in the ear drum), followed by the insertion of grommets – these are small tubes that allow air to pass into the middle ear and equalise pressures.
- Grommets (tympanostomy tubes) fall out on their own and the tympanic membrane self-heals.
References
https://www.nature.com/articles/nrdp201663
https://jamanetwork.com/journals/jamapediatrics/fullarticle/2759422#:~:text=When%20the%20eustachian%20tube%20does,asthma%2C%20and%20seasonal%20allergies).
https://calgaryguide.ucalgary.ca/acute-otitis-media-pathogenesis-and-clinical-findings-in-children/
https://www.ncbi.nlm.nih.gov/books/NBK470332/
https://cks.nice.org.uk/topics/otitis-media-with-effusion/management/management/