Chronic liver disease occurs when the liver is exposed to various insults, resulting in diminishing function over a longer time period. Cirrhosis describes irreversible and long-term damage to the liver due to significant incorporation of scar tissue into the liver architecture.
Functions of the Liver
It can be useful to quickly recap the basic functions of the liver to understand what happens when the liver begins to fail.
- Protein, carbohydrate, and lipid metabolism: The liver is involved in the metabolism of all three of these basic macronutrients.
- Clotting: The liver is responsible for producing fibrinogen, prothrombin, factors V, VII, IX, X and XIII, antithrombin, and many other coagulation factors. Thus
- Bilirubin metabolism: The liver is the main site of bilirubin conjugation
Pathophysiology
An easy way to understand cirrhosis is in three simple steps.
1) Repetitive/chronic injury results in scar tissue.
2) The scar tissue will firstly cause reduced liver function.
3) The scar tissue will result in portal hypertension, which manifests as various signs and symptoms. A more detailed explanation is as follows:
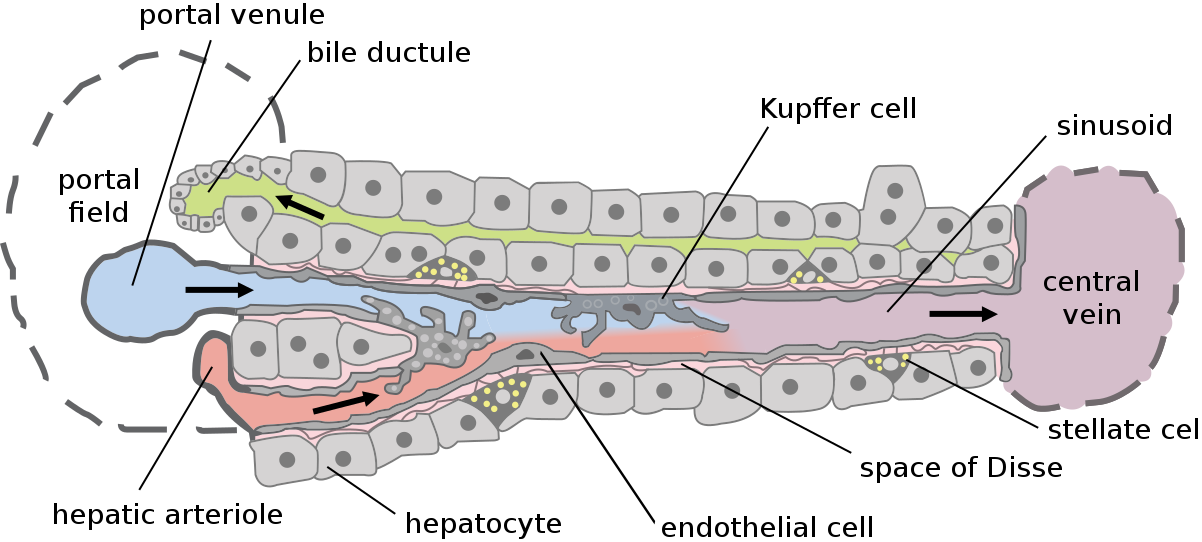
- Chronic injury to the liver e.g., from hepatitis or alcohol abuse leads to hepatocyte damage through apoptosis. Damaged hepatocytes will release damaging reactive oxygen species which activates hepatic stellate cells and tissue macrophages which phagocytose apoptotic cells. They also release inflammatory mediators including transforming growth factor-beta (TGF-b)
- In response to mediators like TGF-b, hepatic stellate cells convert into myofibroblasts and begin depositing collagen i.e., they begin the process of fibrosis.
- Liver sinusoidal endothelial cells are the cells that line the sinusoidal wall i.e. the wall of the small capillaries in the liver that carry blood towards the hepatic vein (which then goes back to the heart). Normally, these cells produce nitric oxide which is a vasodilator and relaxes the sinusoid, and endothelin-1 (ET-1) which is a vasoconstrictor and contracts the sinusoid.
- In cirrhosis, the balance tips towards production of ET-1 and decreased NO production, leading to intrahepatic vasoconstriction which starts the process of portal hypertension.
- The opposite effect happens systemically, and in the splanchnic circulation – there is increased production of NO elsewhere, resulting in systemic vasodilation and decreased systemic vascular resistance.
- Cirrhosis is also associated with increased oestrogen levels due to increased conversion of peripheral androgens into oestrogen.
Originally by Frevert U, Engelmann S, Zougbédé S, Stange J, Ng B, et al. Converted to SVG by Viacheslav Vtyurin who was hired to do so by User:Eug., CC BY 2.5 , via Wikimedia Commons
Hepatic Lobule Structure
Causes
There are a range of causes for cirrhosis including:
Metabolic
- Alcoholic liver disease
- Non-alcoholic fatty liver disease
Viral
Genetic
- Wilson’s Disease
- Alpha-1 antitrypsin deficiency
- Hereditary haemochromatosis
- Cystic Fibrosis
Autoimmune
- Primary Biliary Cholangitis
- Primary Sclerosing Cholangitis
- Autoimmune Hepatitis
Histopathology
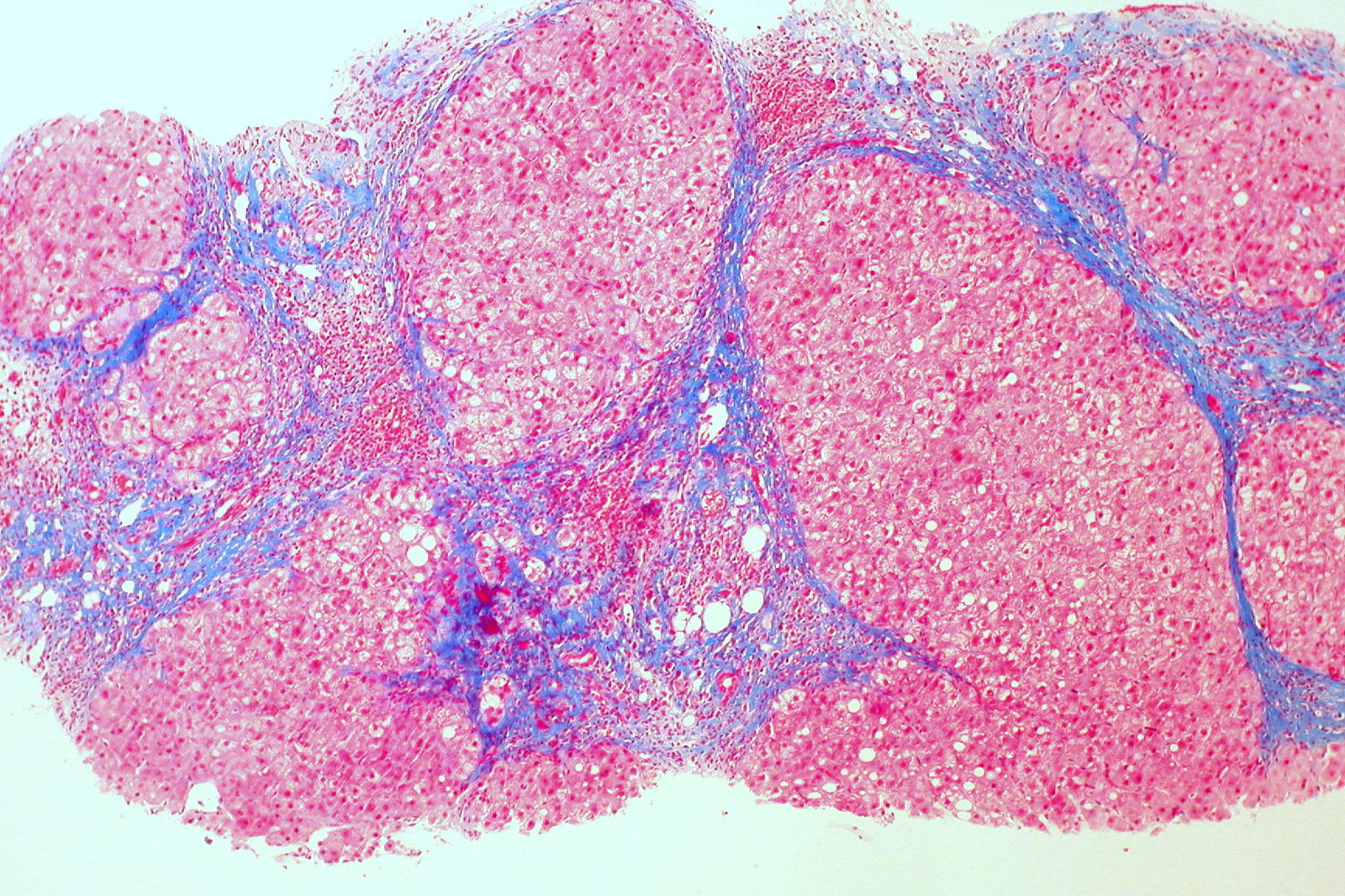
On microscopic examination, there is usually a loss of the normal lobular architecture of the liver. Instead, regenerative nodules are seen, and these are surrounded by fibrous tissue. If these nodules are <3mm, the cirrhosis is described as micronodular, and this is typically seen in alcoholic liver disease and haemochromatosis.
Irregular nodules that are larger than 3mm are given the term macronodular cirrhosis – this is typically seen with hepatitis B, hepatitis C and alpha-1 antitrypsin deficiency.
It is possible to have a mixed micronodular and macronodular pattern as well.
Ed Uthman from Houston, TX, USA, CC BY 2.0 , via Wikimedia Commons
Liver Cirrhosis Microscopy
Here, you can see the collagen in blue i.e. the fibrous septa with regenerating nodules in between.
Clinical Features
You can categorise most signs and symptoms of chronic liver disease into two:
- Portal hypertension
- Hepatic insufficiency
- Oestrogen excess
Portal Hypertension
- Caput medusa: Visibly engorged superficial abdominal veins
- Haemorrhoids
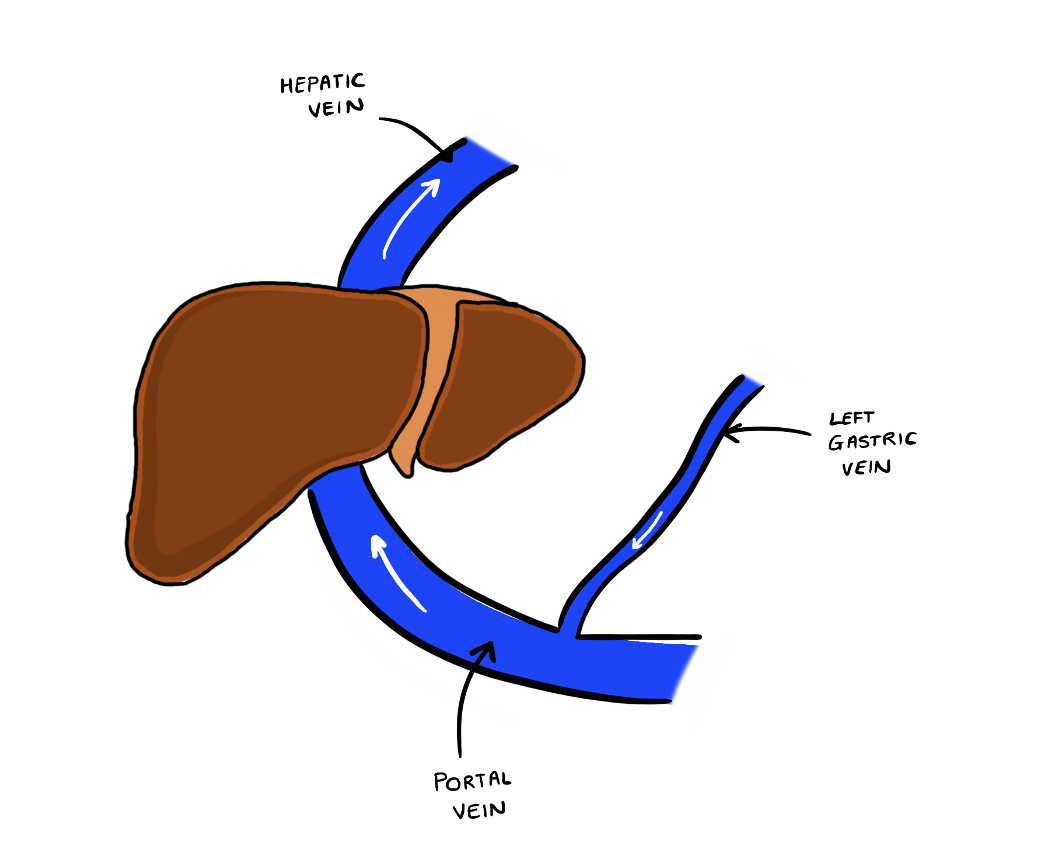
- Oesophageal varices: The veins of the lower third of the oesophagus drain into the left gastric vein, which drains into the portal vein. Raised portal pressures cause a backlog, resulting in dilation of the oesophageal vessels.
- Hepatosplenomegaly
Hepatic Insufficiency
Reduced Protein Synthesis
- Ascites: Build-up of fluid in the peritoneal cavity that can be understood through the ‘overflow and underfill theory’.
- Systemic (and splanchnic) vasodilation reduces systemic vascular resistance and thus the circulating volume
- This activates the renin angiotensin system, leading to sodium and water retention
- This increases hydrostatic pressure and pushes fluid into the interstitial space and peritoneal cavity.
- Oncotic pressures are also low due to insufficient proteins e.g. albumin
- Hepatic encephalopathy: Due to insufficient clearance of harmful waste products such as ammonia which can cause altered levels of consciousness. Asterixis is associated with hepatic encephalopathy (flapping tremor)
- Jaundice: Insufficient conjugation of bilirubin and accumulation of bile salts
- Leuconychia: Sign of hypoalbuminaemia
- Peripheral oedema
Reduced Clotting Synthesis
- Coagulopathy: PT/INR and APTT become prolonged.
Oestrogen Excess
- Palmar erythema
- Spider naevi
- Gynaecomastia
Misc.
- Dupuytren’s contracture: Permanent flexion of finger due to thickened palmar fascia.
- Nail clubbing
Investigations
Bloods
- Liver function tests: Usually deranged but can be normal
- Serum albumin: May be reduced due to decreased hepatic synthetic function
- Clotting screen: Raised PT and INR due to decreased hepatic synthetic function
- FBC: May show macrocytic anaemia due to chronic alcoholism, and may also show a thrombocytopaenia
- U&Es: You may find a dilutional hyponatraemia due to excessive water retention
- Serum alpha-fetoprotein: This can be a marker of hepatocellular carcinoma
- Enhanced Liver Fibrosis (ELF) test: This is a biomarker to assess fibrosis
- Ethanol levels: Particularly useful on admission
- Liver screen: As a newly qualified doctor, you might be asked to put in an order for a ‘liver screen’. This includes things like:
- Alpha-1 antitrypsin levels: Alpha-1 antritrypsin deficiency
- Ceruloplasmin: Wilson’s disease
- HAV, HBV, HCV serology: Hepatitis
- EBV, CMV, HIV: General viral serology for liver disease
- Anti-nuclear antibody (ANA), anti-smooth muscle antibody (aSMA), liver-kidney microsomal antibodies (LKM), anti-mitochondrial antibody (AMA): For autoimmune conditions
Imaging
- Ultrasound: Can be useful, but findings may be non-specific and mimic that of steatosis (fatty liver).
- Transient elastography (FibroScan): Involves passing vibrations through the liver using a non-invasive ‘ultrasound-like’ probe and then measuring how quickly this vibration travels a particular distance through the liver. It is effectively a way of measuring the stiffness of the liver.
- CT and MRI: Can be used for detecting hepatocellular carcinoma
Special Tests
- Liver biopsy: This is the gold-standard method of diagnosing cirrhosis.
NICE Guidelines
UK NICE guidelines mainly use transient elastography or acoustic radiation force impulse imaging for the diagnosis of cirrhosis:
- Transient Elastography: Used for diagnosing cirrhosis in someone with Hepatitis C, people with alcoholic liver disease, men who drink 50+ units of alcohol a week or women who drink 35+ units of alcohol a week
- Transient Elastography OR acoustic radiation force impulse imaging: Used for diagnosing patients with non-alcoholic fatty liver disease and advanced liver fibrosis (i.e. enhanced liver fibrosis or ELF test score >10.51).
Monitoring and Surveillance
UK NICE guidelines state people with a diagnosis of alcoholic liver disease, non-alcoholic liver disease + advanced liver fibrosis, and people with hepatitis C who do not have a sustained response to antivirals should be offered retesting liver cirrhosis every two years.
Patients should also be offered:
- Ultrasound every 6 months: If cirrhosis and no hepatitis B, to check for hepatocellular carcinoma. Serum alpha-fetoprotein may also be measured.
- Upper gastrointestinal endoscopy: Every 3 years to monitor for oesophageal varices.
Management
Management depends on the underlying cause e.g. weight reduction, alcohol cessation, antivirals (viral hepatitis), ursodeoxycholic acid (primary biliary cholangitis) etc. Patients should be encouraged to avoid alcohol, and can be offered vaccination against hepatitis B and C. It is also important to manage the possible subsequent complications.
Some patients may be suitable for liver transplantation – there are specific criteria for qualifying for a liver transplant.
Complications
Child-Pugh Score
The Child-Pugh is a scoring system which is used to establish a prognosis in patients with cirrhosis.
| Parameter | 1 | 2 | 3 |
| Total bilirubin (μmol/L) | <34 | 34-50 | >50 |
| Albumin (g/L) | >35 | 28-35 | <28 |
| PT | <4 | 4-6 | >6 |
| INR | <1.7 | 1.7-2.3 | >2.3 |
| Ascites | None | Mild/Responds to medication | Moderate/Severe/Refractory |
| Hepatic encephalopathy | None | Grade I-II | Grade III-IV |
5-6 points correlates with a 84% one year survival, 7-9 with 62% and 10-15 with a 42% one year survival rate.
References
https://en.wikipedia.org/wiki/File:HRS_and_ascites_pathophysiology.svg
https://www.ncbi.nlm.nih.gov/books/NBK482419/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4064077/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3664283/#__sec2title
https://www.nice.org.uk/guidance/ng50/chapter/Recommendations#diagnosis
https://pubmed.ncbi.nlm.nih.gov/1133151/
https://www.ncbi.nlm.nih.gov/books/NBK430869/
https://emedicine.medscape.com/article/182098-overview#a5
https://www.uhs.nhs.uk/OurServices/Radiology-scansandimaging/PatientInformation/TIPSS.aspx
https://www.racgp.org.au/afp/2013/july/fibroscan/
https://britishlivertrust.org.uk/information-and-support/living-with-a-liver-condition/tests-for-different-types-of-liver-disease/
https://www.exeterlaboratory.com/test/autoimmune-liver-screen/
https://www.ncbi.nlm.nih.gov/books/NBK554597/
https://www.bsg.org.uk/clinical-articles-list/management-of-hepatic-encephalopathy-beyond-the-acute-episode-dr-mcpherson-and-dr-thompson-provides-insight-into-the-management-of-hepatic-encephalopathy/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1904420/
https://www.sps.nhs.uk/wp-content/uploads/2014/05/UKMI_QA_What_is_the_Child-Pugh_score_update_October_2020.pdf