The underlying pathology of myasthenia gravis involves auto-antibodies. In normal cells, an action potential reaches the end of a pre-synaptic neuron and triggers the release of acetylcholine, a neurotransmitter. Acetylcholine binds to nicotinic acetylcholine receptors (nAChR) on the muscle fibre to trigger an action potential and subsequent muscle contraction.
In myasthenia gravis, most patients (roughly 85%), produce antibodies against the nAChRs which causes several problems with nerve transmission.
Ultimately, the antibodies will prevent an action potential forming post-synaptically, effectively removing the trigger that causes muscle contraction.
Anti-Muscle-Specific Kinase (Anti-MuSK)
A smaller proportion of patients with MG will have Anti-MuSK antibodies. MuSK is a receptor tyrosine kinase which is found on the neuromuscular junction with AChRs. Activation of MuSK is important in the functioning of AChRs.
Antibodies to MuSK stops the proper formation of AChRs and will lead to a reduction in the amount of AChRs on the endplate of the neuromuscular junction
Myasthenia gravis is associated with diseases of the thymus gland, particularly thymomas or thymic hyperplasia, suggesting the thymus may also play a role in this condition. Additionally, patients who develop myasthenia gravis may also have pre-existing autoimmune conditions such as rheumatoid arthritis.
Patient with Myasthenia Gravis Exhibiting Ptosis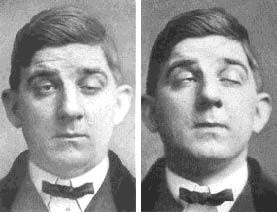
Testing for antibodies is one of the main diagnostic investigations as it will identify the cause. Checking for anti-acetylcholine receptor antibodies is a first-line investigation, followed by checking for serum anti-MuSK antibodies if the former is negative. Due to the association of thymomas/thymic disorders, it may also be beneficial to conduct a CT scan.
Tensilon (or edrophonium) tests are commonly asked about in exams but are not used very frequently in practice due to a danger of bradycardia. The test involves the administration of intravenous edrophonium which is an acetylcholinesterase inhibitor i.e. inhibiting the enzyme which breaks down acetylcholine. A transient improvement in muscle weakness is a positive test.
Electromyography studies (EMG) may also prove to be useful as they can show diminished action potentials in the muscle following repeated nerve stimulation.
The main principle of treatment is to increase the availability of acetylcholine in the synaptic cleft by blocking the enzyme cholinesterase which ordinarily breaks it down. Thus, anticholinesterases such as pyridostigmine can be used to treat myasthenia gravis.
Prednisolone is usually used if patients are not responding to pyridostigmine. Finally, a thymectomy can also lead to improvement, especially in younger patients.
A myasthenic crisis is a complication of myasthenia gravis whereby the condition leads to extremely severe weakness of the respiratory muscles which can lead to respiratory failure. It is crucial to monitor the forced vital capacity (FVC) of a patient in these situations. A myasthenic crisis is typically treated with IV Immunoglobulin or plasmapheresis, the latter of which acts to remove anti-AChR antibodies.
Phillips WD and Vincent A. Pathogenesis of myasthenia gravis: update on disease types, models, and mechanisms. [internet]. 2016. [cited 20thJuly 2019]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4926737/
Sussman J, Farrugia ME, Maddison P, Hill M, Leite IM and Hilton-Jones D. Myasthenia gravis: Association of British Neurologists’ management guidelines. [internet]. 2015. [cited 20th July 2019]. Available from: https://pn.bmj.com/content/15/3/199