Chest x-ray (CXR) interpretation can seem daunting when starting out, but with a systematic approach and practice, spotting lesions becomes easier.
Patient Details, Location and Indication
It is always helpful to ensure you are looking at the CXR for the correct patient, so always start by checking the patient details and the location of the hospital. Furthermore, having an idea as to why the CXR was performed is also useful as you can correlate the CXR findings to the clinical picture e.g. the patient is coughing and has a temperature and the CXR shows signs of a pneumonia.
There will usually be a side marker on the x-ray (e.g. an R for right and L for left) to help you differentiate between the sides.
Checking the Adequacy of the Film
You can use the mnemonic RIP to check if it’s possible to interpret the CXR.
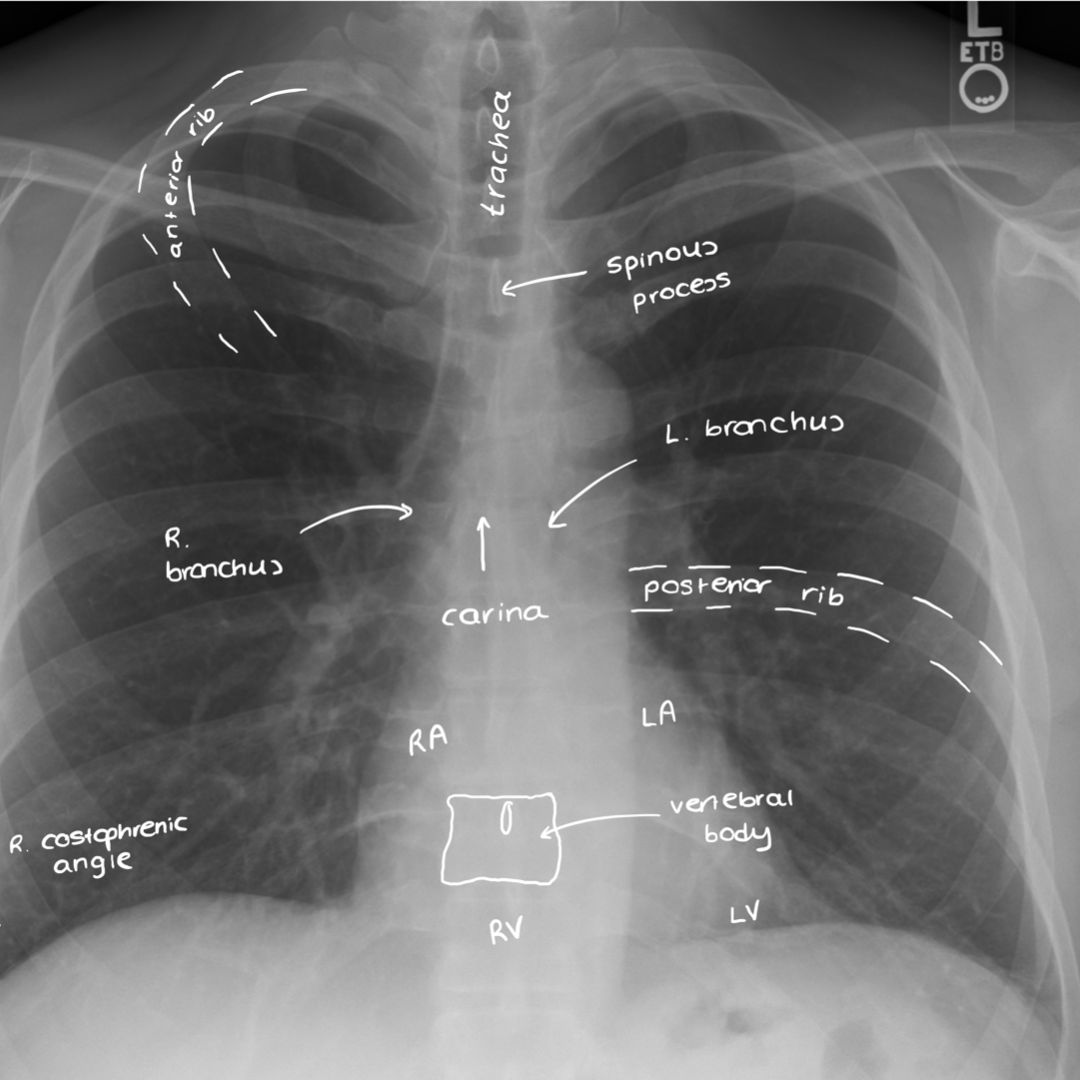
- Rotation: Compare the distance between the heads of the clavicles and the spinous process – are they equidistant? If not, the film is rotated which can make interpretation difficult e.g. assessing deviation of the trachea.
- Inspiration: Should be able to see 6 anterior ribs and 10 posterior ribs for adequate inspiration.
- Penetration: This describes how much the X-rays have passed through the body i.e. penetrated. Can you see the vertebral bodies behind the heart? If not, the x-ray is likely under-penetrated.
CXR Projection
- Posterior-anterior (PA): This is the standard way a CXR is obtained, with the patient standing upright and the x-ray passing from the posterior side to the anterior side of the patient.
- Anterior-posterior (AP): This is the opposite i.e. the x-rays pass from the anterior side of the patient to the posterior side. This is usually done if the patient is too unwell to stand upright (which is helpful to start building a clinical picture of the patient).
The main thing to remember is that you cannot assess cardiomegaly on an AP film because an AP x-ray magnifies the size of the heart.
CXR Terminology
- Lung markings: Lung markings are essentially the hazy ‘vessel like’ opacities you see in the lung fields – it’s basically the lung tissue! If they are absent, it can suggest various things such as a pneumothorax.
- Opacity/density/shadow: Things on an x-ray are referred to as densities or opacities. High density structures or objects are ‘whiter’, such as bone or metal. Lower density structures are ‘blacker’, such as soft tissues, whilst air appears as completely black.
Describing a Lesion
- Where is it? Lung, heart, ribs?
- Which zone of the lung (upper, middle or lower)?
- Number: Are there loads? Is there just one?
- Edge: Well-defined? Spiculating?
- Size: CXR software will usually have a digital ruler than you can use to measure a lesion
- Shape
- Density: Is it metal? Is it calcified? Is it soft tissue?
- Distribution: Widespread? Localised?
- Fluid level: Might suggest an abscess
- Central cavity: Might suggest a granuloma
ABCDE System
The ABCDE system is an easy way to systematically go through a CXR. If you spot a glaringly obvious abnormality from the outset, you can certainly comment on it prior to starting this system. Alternatively, you can use this method if you feel more comfortable doing so.
- Airway
- Breathing
- Circulation
- Diaphragm
- Everything else
Stillwaterising, CC0, via Wikimedia Commons
CXR With Labelled Structures
Airway
- Tracheal deviation?
- Added tubes in the airway e.g. tracheostomy?
Breathing
Lung fields: Start at the apex, go around the chest wall down to the costophrenic angles and then along the cardiac border back to the top, ensuring there are no lesions or abnormalities. Compare both lungs as you do this. You want to be checking the following things:
- Pleura
- Hyperinflation: The diaphragms appear flattened when the chest is hyperinflated.
- Hila
- Mediastinum
- Costophrenic angles
Circulation
- Assess the cardiac shadow. Is the heart enlarged? To determine this, you measure the cardiothoracic ratio. If the heart is more than 50% of the entire chest width, the heart is said to be enlarged.
- Look behind the heart as well
- Is the heart on the correct side? If it is on the right, the patient has dextrocardia, a rare congenital condition.
Diaphragm
- Is there free air under the diaphragm i.e. pneumoperitoneum? If there is, this usually indicates a bowel perforation.
- It can be confusing when you’re first looking at x-rays to tell the difference between a gastric bubble (normal and benign) and a pneumoperitoneum. Gastric bubbles are located in the area you’d expect the stomach to be. Have a look at some chest x-rays of a pneumoperitoneum and some of a gastric bubble and you’ll start to see some differences.
- Are the diaphragms flattened?
- The right diaphragm is normally higher than the left due to the liver.
Everything Else
- Bones: Any rib fractures? Are shoulder dislocations?
- Pacemakers/Internal cardiac defibrillator
- Artificial valves
- Is there surgical emphysema?
- Are there any additional tubes?
Tubes
- ET: The tube tip should lie 5cm above the carina. If it goes too low and into one of the bronchi, the other lung will not get ventilated which can result in a lung collapse, also known as atelectasis.
- Tracheostomy
- PICC: You’ll be able to see a tube which has been peripherally inserted e.g. coming from the side of the arm, and then comes to sit centrally in the heart.
- Central venous catheter: Largely inserted into the right internal jugular vein and sit just over the location of the superior vena cava. If the device is too far into the heart it may cause arrhythmias. Furthermore, sometimes on insertion it is possible to nick the lung going in which can cause a pneumothorax.
- NG: NG tubes should go down the midline, past the carina, across the diaphragm and into the stomach where you should be able to see the tip. The tube should NOT be following the course of the bronchi (you do not want to be giving feeds into the lungs).
- ECG: ECG leads, and stickers may be seen on an x-ray – this can be identified based on the location of the leads/stickers.
- Defibrillator pads
- Oxygen: You may be able to see oxygen delivery tubing on an x-ray.
- Pacemaker
![]()
- Implantable cardiac defibrillator
- Chest drains: If pointing upwards, usually draining a pneumothorax (because air rises up), whilst pleural effusion chest drains usually point downwards.